Everything About Knee Cartilage Damage
As a highly complex and heavily used joint, the knee is essential, enabling key movements like walking, running, jumping, and bending. Central to its seamless function is a specialized tissue that often goes unnoticed until it’s injured: Articular cartilage.
Dr. Rik Kundra, a complex knee surgery specialist in Dubai, frequently helps patients overcome the pain, stiffness, and restricted movement resulting from knee cartilage damage. This damage is not only painful but, if left untreated, can accelerate the onset of severe arthritis.
Dr. Rik believes that understanding your condition is the first step toward effective treatment. This guide will explain what knee cartilage is, how it gets injured, symptoms to watch for, and the advanced treatments available.
What is knee cartilage and why is it important?
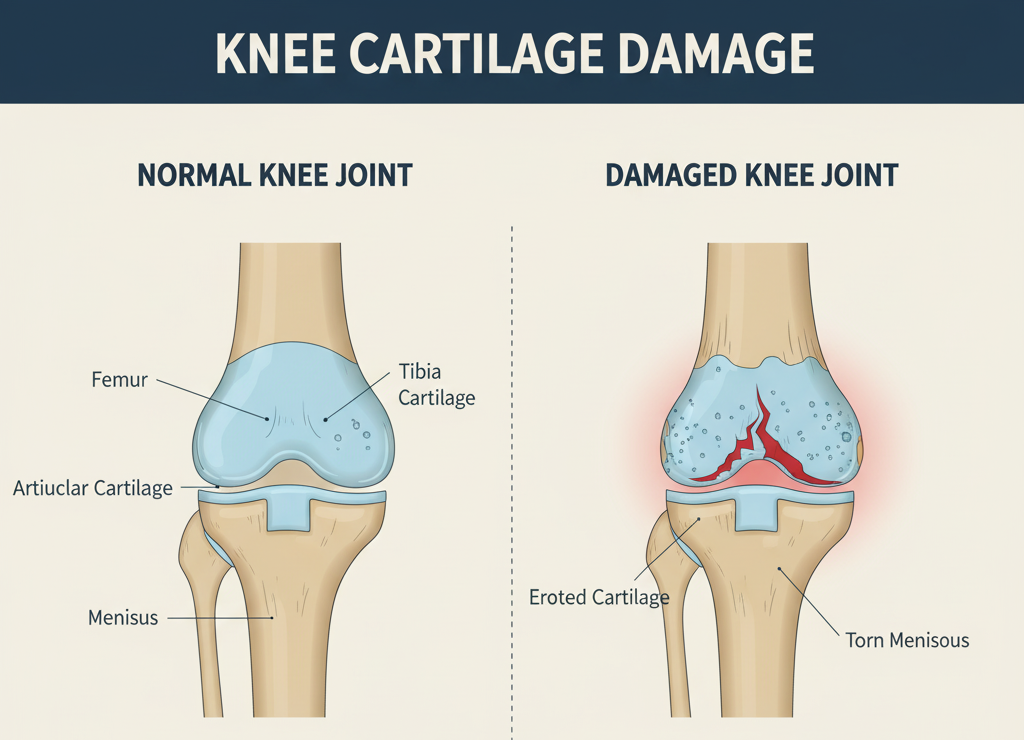
Inside your knee joint, the ends of the thigh bone (femur) and shin bone (tibia) are covered by a thin layer of incredibly smooth, white tissue called articular cartilage. Think of articular cartilage as the natural shock absorber and Teflon coating of your knee. It performs two critical functions:
1- Shock absorption: It cushions the bones, absorbing the impact from walking, running, and jumping.
2- Friction reduction: The primary role of the cartilage is to create a slick surface, enabling the smooth, effortless gliding of bones and eliminating friction.
Unlike many other tissues in the body, cartilage has no direct blood supply. This is key: Because it lacks blood vessels, it has very limited capacity to heal itself naturally once it is damaged.
Causes and types of knee cartilage damage
Damage to this tissue is medically referred to as a knee cartilage injury or chondral lesion. There are two primary ways the damage occurs:
1. Acute injury (Torn cartilage in knee): This usually results from a sudden, sharp trauma, often during sports. A hard pivot, a fall, or a direct blow to the knee can cause a single traumatic event that results in a flap, tear, or even a full-thickness defect in the cartilage.
2. Degenerative wear and tear (Osteoarthritis): This is the most common cause. Age, obesity, or chronic overuse usually cause the cartilage to wear down slowly. This gradual thinning and breakdown of the cartilage surface signals osteoarthritis.

Knee cartilage damage symptoms: How to know you are injured?
The symptoms of a cartilage damage in knee injury can vary depending on the size and location of the lesion, but they often include:
Pain: The pain tends to intensify during activity, particularly with weight-bearing movements such as climbing stairs or performing deep squats.
Swelling: Fluid buildup, or effusion, in the knee joint.
Stiffness: A feeling that the knee is “catching” or tight, especially after sitting for a period.
Catching or locking: The most telltale sign of a torn cartilage in knee flap. When a fragment tears loose, it can become trapped between the moving components of the joint, leading to a temporary locking of the knee.
Grinding or clicking: A sensation of bone-on-bone friction (crepitus) as the smooth cartilage surface erodes.
If you notice these knee cartilage damage symptoms, especially chronic stiffness or repeated catching, see a specialist immediately. This can help prevent further joint deterioration.
Diagnosis: Beyond the X-ray
Patients often ask, “How to know if you have cartilage damage in knee?” The diagnostic process involves a thorough physical exam and sophisticated imaging:
Does a knee X-ray show cartilage damage?
No, a standard knee X-ray does not directly show cartilage damage. Cartilage is soft tissue and does not appear on X-rays. X-rays are excellent for viewing bone structure and alignment.
We use them mainly to look for bone spurs or joint space narrowing—these are indirect signs of advanced cartilage loss and osteoarthritis.
The role of the knee cartilage damage MRI
The gold standard for non-invasive imaging of soft tissues is the MRI (Magnetic Resonance Imaging). A knee cartilage damage MRI gives detailed, cross-sectional images of the cartilage, ligaments, tendons, and meniscus. It can accurately:
- Grade the severity of the cartilage defect (from a shallow lesion to a full-thickness defect).
- It accurately determines the exact size and precise location of the lesion.
- Identify any loose fragments (debris) within the joint.
Arthroscopy
In certain complex cases, a minimally invasive surgical procedure called arthroscopy may be performed. This technique allows direct visualization of the cartilage damage with a small camera and confirms the extent of injury.
Treatment: How to fix cartilage damage in knee?
Since cartilage does not heal itself, intervention is almost always necessary for relief. This also helps protect the joint’s long-term health. The choice of treatment for cartilage damage in the knee depends on factors such as age, activity level, the size of the defect, and overall joint health.
Non-surgical treatment
These options focus on pain relief, swelling management, and slowing the progression of wear:
- Physical therapy: Strengthening the muscles surrounding the knee helps improve overall joint stability and enhances its ability to absorb shock.
- Injections: Corticosteroids for inflammation or Viscosupplementation (Hyaluronic Acid) to improve the joint fluid’s lubricating properties.
- Activity modification: Switching to lower-impact activities and reducing things like running and jumping.
Also Read – What to know about knee injections for osteoarthritis?

Surgical treatment: How to fix cartilage damage in knee?
When conservative treatments fail or the cartilage lesion is severe, surgery may be the best option. It can repair or replace the damaged tissue. As a specialist, I often use advanced, motion-preserving techniques:
Chondroplasty/Debridement: Using arthroscopy to smooth out the frayed edges of the cartilage to prevent catching and irritation.
Microfracture: This technique involves making tiny holes in the underlying bone to stimulate a blood clot. This clot forms a type of scar tissue (fibrocartilage) that fills the defect. It is best used for smaller defects.
Autologous chondrocyte implantation (ACI): This two-stage procedure involves harvesting healthy cartilage cells from the patient, culturing them in a laboratory, and then re-implanting the multiplied cells into the knee defect.
Osteochondral autograft transfer (OATS/Mosaicplasty): Taking small, healthy plugs of bone and cartilage from a non-weight-bearing area of the knee and transferring them to the damaged site.
Partial or total knee replacement: This is reserved for cases of widespread, end-stage arthritis. It is used where the damage is too extensive for cartilage repair techniques.
Take the next step for your knee health
Addressing knee cartilage damage requires specialized expertise. Delaying treatment may lead to further joint damage and fewer treatment options over time.
Dr. Rik Kundra is dedicated to accurately diagnosing your condition and providing the most advanced, individualized treatment plan, whether through conservative management or surgical restoration.
Don’t let knee pain define your activity level. Contact us today to schedule your consultation and explore the best treatment options available for achieving lasting pain relief and restoring your full mobility.
Disclaimer
All content and media on this page are created and published for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Meet Dr. Rik personally for appropriate medical diagnosis and advice.


